In the world of retinitis pigmentosa (RP), it’s crucial to grasp its two primary classifications: non-syndromic and syndromic. This distinction lays the foundation for understanding the condition’s complexity and its implications for affected individuals and their families.
Non-Syndromic Retinitis Pigmentosa: The Majority
Comprising a substantial 70-80% of RP cases, non-syndromic RP presents without associated systemic abnormalities. In essence, it primarily manifests within the eye without involving other bodily systems. However, its impact on vision and overall well-being can be profound.
Syndromic Retinitis Pigmentosa: Beyond the Eye
Contrastingly, syndromic RP accounts for 20-30% of cases and is characterized by additional non-ocular syndromes and systemic diseases. This form of RP presents a more intricate clinical picture, often requiring a multidisciplinary approach for management and treatment.
For any queries, feel free to reach us @ https://www.towardshealthcare.com/personalized-scope/5114
Genetic Landscape of Non-Syndromic RP
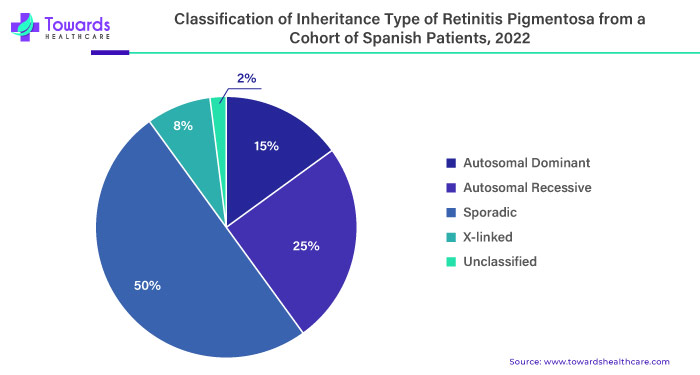
The genetic underpinnings of non-syndromic RP are diverse and intricate, with mutations in approximately 80 different genes implicated. These mutations can follow various inheritance patterns, including autosomal recessive, autosomal dominant, and X-linked recessive, each contributing to the complexity of the condition.
Insights from Research: Unveiling the Complexity
Recent studies, such as one conducted in Spain in 2021, shed light on previously overlooked aspects of RP. For instance, while X-linked RP was traditionally believed to predominantly affect males, emerging evidence suggests that female carriers can exhibit a spectrum of symptoms, ranging from asymptomatic to severe retinal disease.
The Sporadic Cases: An Enigma
Amidst the well-defined genetic landscape of RP lies a category of cases deemed “sporadic.” These cases present without a clear inheritance pattern or molecular mechanism, posing a challenge for researchers and clinicians alike in understanding their etiology and management.
Impact on Quality of Life
Beyond the genetic and clinical intricacies, RP’s true significance lies in its profound impact on individuals’ quality of life. Vision loss, a hallmark of RP, can impede independence, mobility, and overall well-being, underscoring the urgency of effective management and treatment strategies.
Addressing the Growing Need
As highlighted by the CDC’s revelations in 2023, the prevalence of vision impairment, including RP, underscores the growing need for innovative treatments and technologies. With an aging population and increasing awareness of genetic diseases, there’s a burgeoning demand for precision medicine and gene therapy to address RP and similar conditions.
Promising Therapeutic Avenues
The landscape of RP treatment is evolving rapidly, buoyed by advancements in gene editing, stem cell therapy, and retinal implants. These innovative approaches offer hope for restoring visual function and improving outcomes for individuals affected by RP, driving optimism within the scientific and medical communities.
Navigating the Treatment Market
The burgeoning market for RP treatments and technologies reflects the increasing investment in research and development by various stakeholders. From biotech and pharmaceutical firms to academic institutions and government bodies, efforts are underway to accelerate the translation of scientific discoveries into viable therapies.
Unlock Infinite Advantages: Subscribe to Annual Membership
To own our research study instantly, Click here @ https://www.towardshealthcare.com/price/5114
Read More about Retinitis Pigmentosa Market: